Abstract
The mechanisms of T cell-dependent tolerance, especially its signaling pathways after haploidentical hematopoietic stem cell transplantation (haplo-HSCT), are incompletely understood. Both central and peripheral regulation mechanisms are suspected.
Subjects and Methods: We tested 8 patients with leukemia (5) or myelodysplastic syndromes (MDS, 3) (age 35-73-years old, median: 51-years old) following IRB approved consenting. All received Flu+TBI (+/- Cy) pre-conditioning and haplo-HSCT with post-transplant Cytoxan (PTCy) and FK506 as GvHD prophylaxis. Chimerism at tolerance studies was donor dominant (97-100%, mean: 99% for both CD33+ myeloid cells and CD3+T cells). Immunosuppression drug (ISD) was withdrawn ~6 months before the time of the in vitro tolerance study described below.
We described previously Treg depletion from purified T cells with IL2-immunotoxin (Denileukin Diftitox, Seragen Inc™) to test the involvement of these cells in long-term tolerance. The contribution of Tr1 or anergy was examined by either blocking IL10R or adding low dose IL2, respectively. T-cell exhaustion was tested by blocking the PD1 pathway with anti-PD1 MoAb (OPDIVO, Bristol Myers Squibb™). Purified T cell responses to recipient dendritic cells (DC) were measured in mixed lymphocyte reaction (MLR) assay, and further tested by quantifying cytokine secretion in MLR culture supernatants using Bio-Plex immunoassays (Bio-Rad Lab™). To test for clonal deletion, alloreactive T-cell clones with frequency >0.1% identified in vitro from the graft pre-infusion were tracked by monitoring their T-cell receptor CDR3 sequence serially, in an ImmunoSEQ™ assay (Adaptive Biotech™). Gene expression profiling and signaling pathway analysis on alloreactive or tolerant T-cells were performed by collecting T cells from in vitro MLR reactions, purifying total RNAs from these cells, running RNA-sequencing and analyzing with software of CLC Genomic Workbench®v21, GSEA®v4.1.0 and IPA®.
Results: We have previously shown that circulating T cells were hyporeactive to recipient DC in patients at 1yr (or 2yrs in 1 patient) post-haplo-HSCT [6 months, (or 2-5 months in 3 patients) post-ISD withdrawal], while these T cells responded vigorously to 3rd party APC, As positive control, host DC triggered robust 3rd party T-cell response. Neither depletion of Tregs, nor blockade of IL10R or PD1 could reverse T-cell hypo-reactivity. Low-dose IL2 triggered mild anti-host proliferation responses. Similar scenarios were detected in graft T cells against self-DC, (negative control in autologous set up), while vigorous responses were shown in the graft T cells against host-DC pre-haplo-HSCT. Cytokine profiling further confirmed the MLR responses. ImmunoSEQ™ revealed disappearance of alloreactive T-cell clones from peripheral blood with time. Low dose IL2 had minimal impact to reverse hyporeactivity. While most alloreactive T clones were undetectable, a few remained in the peripheral pool in tolerant patients tested (Nee, T et al, Transplantation and Cellular Therapy, 2022;28(3):S44-S45).
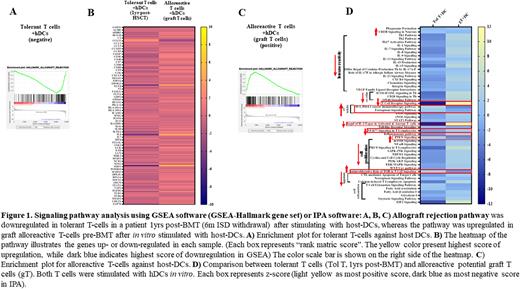
Unlike graft T-cell responses against host DC, tolerant T-cells in circulation (including remaining alloreactive T cells) against hDC showed distinct patterns of gene expressions, with relative downregulation of allograft rejection (GSEA-Hallmark) (Fig 1A, B, C) and T-helper response, co-stimulation, cell proliferation pathway, that was paired with upregulation of co-inhibition, PD1-PDL1, Ferroptosis, PTEN and CREB pathways (Fig1D). The profiles suggested systemic alterations in the signaling pathways on tolerant T cells post-haplo-HSCT.
Conclusion: Hypo-reactivity of donor-derived circulating T cells to recipient DC and graft T cells to graft DC (negative control) were evident. We found Treg, Tr1 activity or T-cell exhaustion to be insignificant as their blockade or removal did not lead to 'flare’ in circulating tolerant T-cell reactivity against patient DC. T-cell clonal deletion appears to be the dominant mechanism explaining the in vitro hyporeactive proliferation, cytokine secretion, and alloreactive TCR clonotype attrition, along with systemically altered signaling pathways in tolerant T-cells including the alloreactive T cells remained. Anergy may play a minor supportive role.
Disclosures
Szabolcs:Forge Biologics, Inc: Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal